The Research Track
The Research Track is one of four available Tracks. Residents in the Research Track can select mentors from across the entire UCLA campus, representing a broad range of expertise including basic, clinical, translational, health services, and social sciences. Research Track leadership can help to identify and introduce junior residents to prospective research projects and faculty mentors.
Benefits of the program include protected time from clinical duties to focus on research-related activities and internal funding opportunities during the PGY-3 and PGY-4 years through the UCLA-Semel Psychiatry Research Catalyst Award. The program curriculum also provides regular opportunities to meet leading researchers and clinicians in psychiatry and learn about their areas of interest during regular lunchtime forums. The lunch forum also involves journal club discussions led by residents on cutting-edge topics in psychiatry and oral presentations given by residents on their research projects.
Beyond the residency training period, the program is committed to supporting residents as they pursue their research career interests. Mentorship and guidance continue after residency and there are a wide variety of post-residency research opportunities. The UCLA and the VA system offer research fellowships, a child psychiatry fellowship research track, and numerous post-doctoral positions.
Even if you are not formally in the Research Track, you can still participate in research! Residents in the Mid-Wilshire, Greater Los Angeles, and Westwood Tracks who are interested in pursuing research activities during residency can apply for up to 30% protected time for their projects during PGY-3 and 4.
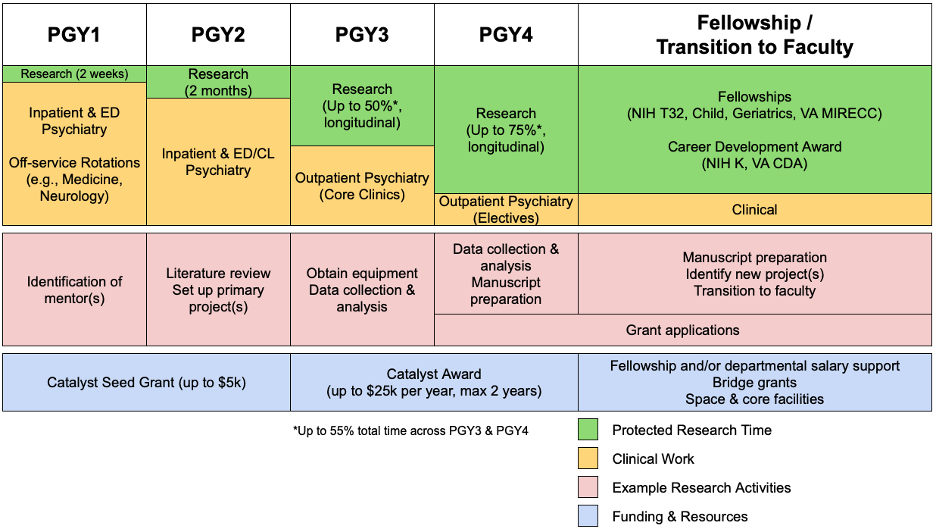
Residents in the Research Track will receive protected time to engage in research during all four years of residency training.
In PGY-1, this takes the form of 2 weeks to help identify a research mentor.
In PGY-2, two clinical blocks (approximately 8 weeks) are set aside for research. Scheduling is flexible and will be done in coordination with the Residency Education Office to maximize the benefit for each resident (such as placing this time at the end of PGY-2 to facilitate the transition to more intensive research in PGY-3 and 4).
In PGY-3 and 4, Research Track residents are granted protected time for research while meeting ACGME clinical requirements and attending didactics. On average, residents have up to 55% of their time protected for research across the two years. This protected time can be flexibly divided between PGY-3 and 4, so that residents can assign more protected time during their PGY3 (up to 50%) or PGY4 (up to 75%) years.
Applicants to the Research Track should have an established record of outstanding research accomplishments. It is anticipated that most will have obtained an M.D./Ph.D. degree. Engagement in an equivalent amount of extensive and rigorous research training may be acceptable in some cases.
To apply, medical students must check the box for program NRMP 3030400C1 on their application. In addition to the standard ERAS application, the following components are required:
• A letter of recommendation from a former and/or current research mentor.
• Research Track Secondary Application (which will be sent out shortly after we receive your ERAS Application).
Invitations to interview for the Research Track will be sent by email. Notified applicants will attend an additional day of interviews to meet with potential research mentors and members of the Research Track committee. This is normally coordinated with Residency Education to occur the same week as interviews for the Categorical Residency. However, a separate day for interviews with potential mentors may be arranged if needed.
The Director and Residency Education Staff will be responsible for coordinating the interviews.
Research Track (RT) residents are uniquely eligible for an internal funding opportunity through the UCLA-Semel Psychiatry Research Catalyst Award. This award provides up to $25,000 per year for up to two years (a total of $50,000 per resident) to support the development of rising PGY-3 and PGY-4 RT residents into successful, independent investigators in psychiatry. Funding can be applied to research-related costs including equipment/supplies, consultant fees, software, travel, coursework, and more.
Alternatively, RT residents in earlier stages of training may apply for the Catalyst Seed Grant which provides off-cycle funding (<$5,000) for special and/or unanticipated circumstances.
- Funded, flexible, protected time during PGY-1 (2 weeks), PGY-2 (approx. 15%), and PGY-3/4 (approx. 50-60%) for research (see ‘Protected Time’)
- Exclusive, internal funding opportunities (up to $25,000 per year, up to two years, per resident) through the UCLA-Semel Psychiatry Research Catalyst Award (see ‘Research Funding’)
- Flexible opportunities for fellowships for additional research years across both UCLA and the VA
- Yearly Research Training Retreat at UCLA
- Invitation to yearly VA-sponsored regional research conference
- Flexibility for a customized training path
- Outstanding faculty and training environment
- A collaborative and supportive research community
- Program responsive to feedback and committed to continuous improvement
- Social & networking events
- Career mentorship and guidance
Class of 2026
Dr. Chelsea Shannon is a fourth-year psychiatry resident at UCLA. She attended Stanford University for her undergraduate degree and Dartmouth Geisel School of Medicine for medical school. Her interests include reproductive psychiatry, health systems research, and mental health policy advocacy.
Class of 2027
Dr. Kaleab Tessema received his MD and PhD from UCLA. His thesis work with Dr. Harley Kornblum focused on examining molecular mechanisms underlying 1) neurodevelopmental risk factors for psychiatric conditions (ASD, schizophrenia, bipolar disorder) and 2) progression and recurrence of high-grade glioma. Prior to medical school, Kaleab studied biomedical engineering at Yale University and pursued research projects related to stem cell genetics, HIV reactivation dynamics, artificial muscle generation, and neutrophil transmigration. Moving forward, he is interested in studying childhood trauma/stress or variables driving heterogeneity in clinical response to psychiatric interventions.
Dr. Lauren Textor received her MD and PhD from UCLA. During her PhD in anthropology, she worked with Dr. Philippe Bourgois and Dr. Helena Hansen to examine health systems and federal policies implemented in response to the U.S. overdose epidemic, documenting long-term impacts of these policies for individuals who use opioids. Observation of clinical encounters, mundane bureaucratic processes such as prescription monitoring and pharmacy oversight revealed the encroachment of drug law enforcement into clinical care and abandonment of vulnerable patients. She examines how political economic competition between different models of addiction shapes individuals’ embodiment of addiction and of treatment. She is interested in pursuing anthropological research at the intersection of community organizing and health policy.
Class of 2028
Dr. Hannah Connolly received her MD/MPH from SUNY Upstate Medical University and her PhD in Social Science from the Maxwell School at Syracuse University. Her dissertation explores the professional identity formation of medical students, paying particular attention to their socialization around addressing the social and structural determinants of health. Through a year-long ethnography with third-year medical students, her research illuminates the process of social reproduction upholding a medical student culture of “don’t rock the boat” which directly opposes social justice-oriented curricula. Overall, her research is oriented to medical education transformation through structural competency. She is passionate about interdisciplinary collaborations, participatory-action research, and medical education leadership and curricular reform.
Dr. Will Schlesinger received his MD and PhD from UCLA. His doctoral research in anthropology investigated the successes and shortcomings of pre-exposure prophylaxis (PrEP) to HIV. He conducted ethnographic fieldwork within a broader public health study, led by Dr. Nina Harawa, designed to promote PrEP access and adherence among men who have sex with men (MSM) and transgender women with histories of substance use disorder and recent incarceration. In residency and beyond, Will is interested in continuing to pursue anthropological research at the intersection of mental health and sexual health with a specific focus on queer and transgender patient populations.
Class of 2029
Dr. Zack Blumenfeld received his MD from Keck School of Medicine of USC and PhD from Caltech. His PhD research involved the study of the pharmacokinetics of neuropsychiatric compounds in both cell culture and animal models using novel drug-specific sensing fluorescent reporters in the labs of Profs. Henry Lester and David Prober. As a pre-doctoral RA, he studied deep brain stimulation in Parkinson’s disease patients at Stanford. His current research interests involve the diagnosis and treatment of psychosis, specifically for early onset and first break populations.
Dr. Zachary “Zack” Williams received both his MD and his PhD in Neuroscience from Vanderbilt University. His thesis work, supervised by Tiffany Woynaroski (Hearing & Speech) and Carissa Cascio (Psychiatry) characterized the poorly-understood symptom of “sound sensitivity” (decreased sound tolerance), its subtypes, and correlates in autistic and non-autistic adults. His current research focuses on the intersection of autism and health and disability over the lifespan, including how autism-associated (mental and physical) health issues can be better measured, assessed, and supported or treated by our current health care systems. As a physician-scientist, he seeks to specialize in the overlap of autism with severe/persistent mental illness, working to develop evidence-based treatments and care pathways for autistic adolescents and adults with catatonia, psychosis, bipolar disorder, and other severe and refractory mental health conditions, who are far too often underserved.